Dissociative identity disorder is sometimes confused with schizophrenia, but the two are very different, albeit equally severe, mental health disorders.
To understand dissociative identity disorder in teens, what it looks like in teenagers, and how to treat it, we need to understand dissociation and why it happens.
Dissociative Identity Disorder is a Fragmented Psyche
Dissociative identity disorder, or DID, used to be called “multiple personality” disorder. While fragmented personas and “alters” are still a common element in cases of DID, it’s important to emphasize that our understanding of DID is not centered around the idea of multiple people in one body but a fragmented psyche, usually as the result of a traumatic event.
A significant factor in the development of DID is childhood trauma, with many individuals having experienced childhood abuse, which often leads to their dissociation.
Dissociation is the Main Characteristic
The central characteristic of dissociative identity disorder is dissociation, usually in response to a traumatic event. Dissociation is characterized as a separation or distancing between a person and their perspective on reality.
In one example of dissociation, a person might “check out” in moments of stress, appearing nonresponsive or different somehow. When they’re “back,” they might have no recollection of dissociating or even experience holes in their memory.
In cases of dissociative identity disorder, a person’s dissociation extends to the degree that they become someone else for a while.
Dissociative Identity Disorder vs Psychosis
It is not necessarily the same as psychosis, where a person’s perception of reality is altered significantly through delusions or hallucinations; however, the outside similarities between the two – in the sense that people who dissociate and people who experience psychosis are not entirely present – is what often leads people to conflate conditions like schizophrenia or post-traumatic stress disorder with split personalities or dissociative disorders.
Underdiagnosed or Mistaken for Something Else
As a result, mental health professionals believe that dissociative personality disorder is currently underdiagnosed and may be mistaken for another similar mental health condition.
Currently, about 1 percent of the general population experiences dissociative identity disorder, with rates being significantly higher in clinical settings.
Dissociation as a Defensive Mechanism
In a way, dissociation can be understood as a defensive mechanism after a significantly traumatic event, often rooted in childhood trauma. People who dissociate do so to protect themselves from the reality of their situation and their circumstances.
Dissassotive Symptoms and Trauma
However, these dissociative symptoms can last for a long time and continue to impact a person’s mind even long after the original danger has passed. This is the prime characteristic of trauma – like mental scarring; trauma means reacting, unknowingly and unwittingly, as though the past is recurring or as though what happened is always imminent.
Childhood Trauma and the Development of Dissociative Identity Disorder
Childhood trauma, in particular, plays a crucial role in the development of dissociative identity disorder (DID), with many individuals having experienced childhood abuse as the root cause of their dissociation.
Not everyone dissociates after trauma – dissociation is just one of the ways in which the mind might react to something horrifying or impactful.
Definition and Diagnosis
Dissociative identity disorder (DID), formerly known as multiple personality disorder, is a complex mental health disorder characterized by the presence of two or more distinct identities or personality states within an individual.
These distinct identities, often referred to as “alters,” can have their own unique thoughts, feelings, and behaviors.
Dissociative Amnesia
One of the hallmark features of DID is dissociative amnesia, where individuals experience a loss of memory for important personal information and everyday events. These memory gaps are not due to ordinary forgetfulness but rather a defense mechanism in response to trauma.
Individuals may be unable to recall significant life events, such as childhood experiences, traumatic incidents, or even conversations that took place moments earlier. The amnesia can be localized to specific time periods or more generalized, affecting large portions of a person’s life. This can lead to confusion, distress, and difficulties in maintaining relationships or daily responsibilities.
DSM-5 Criteria for DID Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), outlines the criteria for diagnosing DID. According to the DSM-5, the presence of two or more distinct identities or personality states, along with dissociative amnesia and significant distress or impairment in functioning, are key indicators of DID.
American Psychiatric Association for DID Diagnosis
The American Psychiatric Association emphasizes that diagnosing DID should be left to licensed mental health professionals, as the symptoms can be intricate and may overlap with other mental health conditions.
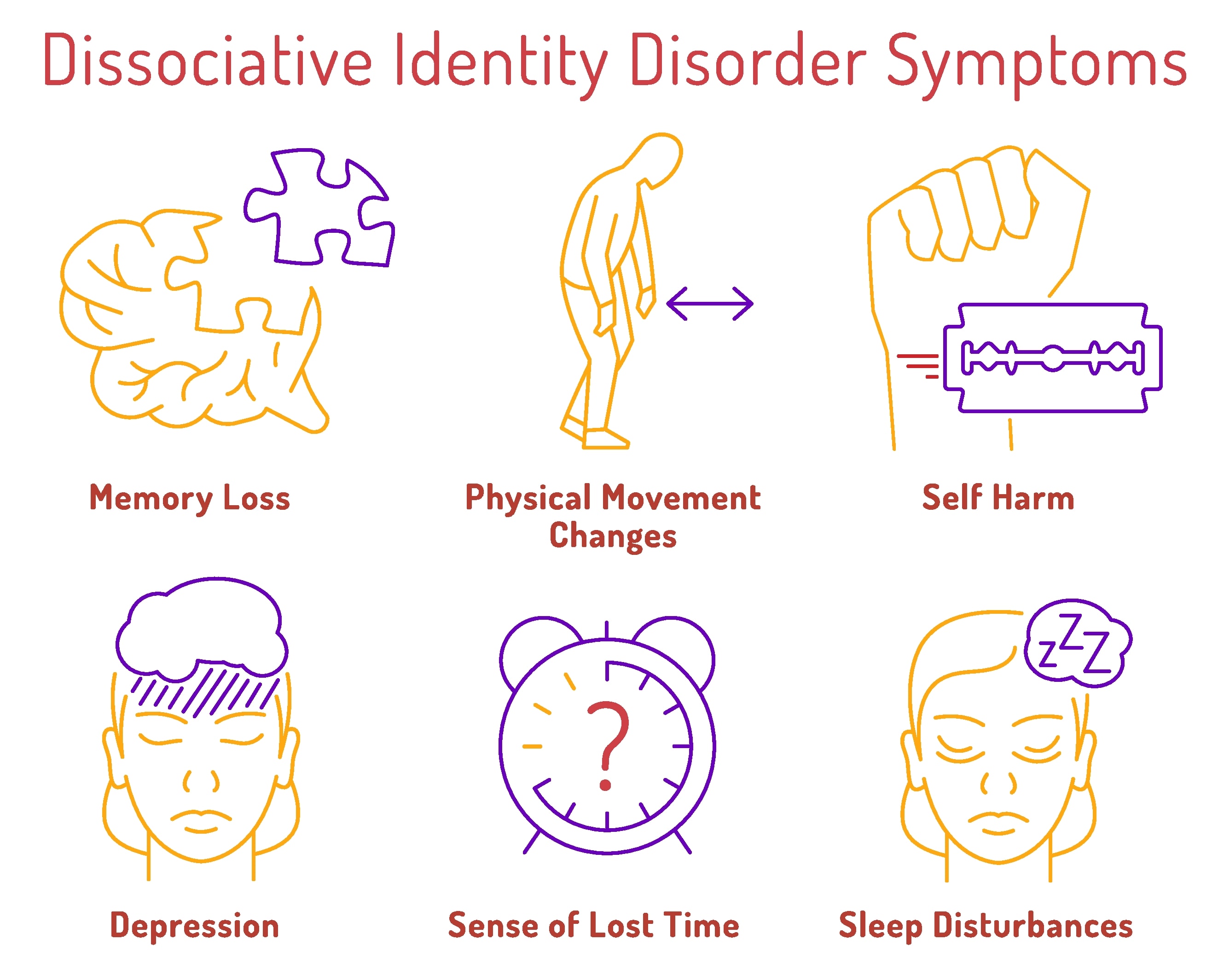
Signs and Symptoms of Dissociative Identity Disorder in Teens
Recognizing dissociation in our loved ones is essential because teen dissociative disorder treatment is effective but takes time and patience to work.
Helping someone heal from their trauma, cope in healthier ways, and develop a consistent and unified personality can help them avoid the negative consequences of dissociative identity disorder, including memory loss, social anxiety, depressive thoughts, and mood swings.
Teens with dissociative identity disorder don’t behave like stereotypes from movies. There is a spectrum of symptoms involved in cases of DID, and not every case is alike. While representations of DID in media have improved in recent years, it’s crucial to differentiate reality from fiction.
Some common signs of dissociative identity disorder in teens include:
1. Separate and Distinct Identities
The defining symptom of dissociative identity disorder is the presence of two or more distinctly different personality states.
These alternate identities, commonly referred to as alters, can vary significantly in terms of age, name, gender, mannerisms, speech patterns, and even physical abilities or medical conditions. Some alters may be more dominant, while others remain in the background, only emerging in specific situations.
In many cases, people develop multiple different personalities, sometimes upwards of five or more. Each alter has its own set of memories, emotional responses, and thought patterns. This can create a complex and fragmented sense of self, making it difficult for individuals with DID to establish a consistent identity. Some alters may be more childlike, while others take on protective or authoritative roles, often shaped by the individual’s past trauma.
Switching from one alter to another may occur randomly. However, it is more common for these transitions to happen in response to a specific stressor. Triggers such as trauma reminders, emotional distress, or even substance use can prompt an abrupt shift between identities. These switches can be disorienting and may result in periods of confusion, memory loss, or emotional distress.
Alters usually do not share memories and may not always be aware of each other’s existence. This means that teens with dissociative identity disorder often suffer from memory gaps and frequent bouts of amnesia. A person with DID may find themselves in unfamiliar places with no recollection of how they got there, or they may struggle to recall important personal details.
Over time, this can lead to significant distress, making daily life, relationships, and academic performance particularly challenging.
2. Memory Issues and Dissociative Amnesia
In addition to changing personalities, accompanying memory problems are another common aspect of dissociative identity disorder.
Teens affected by DID are not acting out as other people – their mind compartmentalizes moments in time, experiencing them as different individuals and not always letting these experiences interact with each other.
Let’s think of dissociation as a protective mechanism. We can imagine it like a series of filters – swapping one filter for another, sometimes in response to a person’s surroundings. Hence, the “right” filter captures the experience, rather than having one filter experience everything simultaneously.
As a result of these swaps, however, teens with dissociative identity disorder might not have a coherent understanding of their day-to-day.
3. Intrusive or Unwanted Thoughts
Intrusive or unwanted thoughts are, to a degree, normal.
We all experience a fleeting moment of thinking about something we did not want to think about or were surprised to think about. However, some mental health conditions can exacerbate the frequency and severity of these thoughts to the point that they almost feel compulsive.
Dissociative identity disorder can cause persistent and distressing unwanted thoughts, usually in the form of recurring memories or flashbacks, sudden traumatic remembrances, or unwanted shifts in thinking, such as an outburst of anger or sadness. These thoughts can emerge without warning and may be tied to past traumatic experiences that contributed to the development of DID. The intrusive nature of these thoughts can make daily life challenging, disrupting focus, sleep, and emotional stability.
Additionally, different identities or alters may struggle with conflicting thoughts, leading to internal turmoil. One identity may experience distressing memories, while another may attempt to suppress or ignore them, creating a cycle of emotional turbulence.
Some intrusive thoughts may not even feel like they belong to the individual, making them even more unsettling. Over time, repeated exposure to these thoughts can heighten anxiety, trigger dissociative episodes, or contribute to feelings of helplessness.
Therapeutic interventions such as grounding techniques, cognitive-behavioral strategies, and trauma-focused therapy can help individuals with DID manage and reduce the impact of intrusive thoughts.
4. Depersonalization and Derealization
Depersonalization and derealization are common symptoms experienced by individuals with dissociative identity disorder.
Depersonalization involves a feeling of detachment from oneself as if observing oneself from outside the body. On the other hand, derealization is characterized by a sense of detachment from the surrounding world, making it feel unreal or dreamlike. These symptoms can be profoundly distressing and interfere with an individual’s ability to function in daily life.
Triggers for depersonalization and derealization often include traumatic events, stress, or anxiety. Other dissociative symptoms, such as dissociative amnesia and identity fragmentation, may also accompany these symptoms.
Treatment for depersonalization and derealization typically involves psychotherapy, with cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) being particularly effective. These therapeutic approaches help individuals manage their symptoms and improve their overall mental health, providing them with tools to navigate their daily lives more effectively.
4. Childhood Trauma
Dissociative identity disorder can be a very socially disabling condition. It is difficult for people to manage friendships and relationships while struggling with DID, and poor experiences can further feed a growing sense of social anxiety as a result of these symptoms.
These anxious thoughts can trigger and worsen traumatic stressors and make the mind more sensitive to such stressors. For teens with DID, social interactions can feel overwhelming, unpredictable, or even dangerous, particularly if past trauma involves interpersonal abuse.
As a result, they may struggle to form and maintain close relationships, experience heightened sensitivity to rejection or perceived criticism, or withdraw from social situations altogether.
Some personalities within a teen may be more confident than others, but social anxiety is still a common symptom. Certain alters may be more extroverted or outgoing, while others remain withdrawn or fearful. This variation in personality traits can make it difficult for a teen with DID to establish a stable social identity, further complicating their ability to interact with peers.
Additionally, they may struggle with trust issues, as their past experiences have conditioned them to expect harm or betrayal. Childhood trauma not only increases the risk of developing dissociative symptoms but can also lead to a range of co-occurring mental health conditions.
Many teens with DID experience symptoms of post-traumatic stress disorder (PTSD), depression, and anxiety, all of which can compound their difficulties in social settings. Traumatic memories may surface unexpectedly, causing intense emotional distress and reinforcing avoidance behaviors. Without proper treatment, the cycle of trauma, dissociation, and social impairment can persist well into adulthood.
However, with early intervention, trauma-informed therapy, and a supportive environment, teens with DID can develop healthier coping mechanisms, build self-confidence, and learn to navigate relationships more effectively.
5. Depressive Symptoms
Depressive symptoms, including symptoms of self-harm and suicidal ideation/suicidal attempts, are also unfortunately common in cases of DID. Furthermore, reports indicate that as many as 70 percent of patients in treatment for DID attempt suicide at one point or another, meaning the unknown statistic may be even higher.
Depression in teens with DID can manifest in various ways, including persistent sadness, feelings of emptiness, emotional numbness, and extreme fatigue. Due to the nature of dissociation, some alters may experience these symptoms more intensely than others, leading to fluctuations in mood and making it difficult for individuals to recognize or express their distress.
Additionally, memory gaps and amnesia between personalities can make it challenging for teens to recall moments of crisis, increasing their risk of self-harm or suicidal behavior without fully understanding why they feel this way.
The weight of unresolved trauma, combined with social isolation and difficulties in maintaining a stable sense of self, can deepen feelings of hopelessness. Many teens with DID also experience co-occurring disorders, such as PTSD and anxiety, further compounding their struggles.
Without proper intervention, depressive symptoms can worsen over time, making comprehensive, trauma-informed treatment essential.
Therapy, medication, and strong support systems can help teens with DID manage their depression, develop healthier coping mechanisms, and reduce their risk of self-harm or suicide.
Related: Teen Depression Treatment
6. Substance Use
Dissociative identity disorder correlates strongly with substance use, at times as a form of self-medication or just for recreational purposes.
Teens with DID may turn to drugs or alcohol as a way to numb emotional pain, escape traumatic memories, or manage the distress caused by their dissociative symptoms. Since different alters can have distinct attitudes toward substance use, some may actively seek out drugs or alcohol, while others may be unaware of or resistant to such behavior.
Sadly, drug use can further amplify the effects and symptoms of DID, as well as suicidal ideation, depressive thinking, and anxiety. Substance abuse can worsen memory blackouts, increase the risk of dangerous behaviors, and make it even more difficult for individuals to maintain control over their actions.
Additionally, withdrawal symptoms and cravings can intensify mood swings and emotional instability.
Early intervention and trauma-focused therapy are essential to help teens with DID address the root causes of their substance use and develop healthier coping mechanisms.
Treating Dissociative Identity Disorder in Teens
Patients with dissociative identity disorder may require outpatient or inpatient residential treatment to see long-term success. In addition to their dissociative and trauma-related symptoms, teen patients with DID may struggle with suicidal thoughts, drug use, and anxiety.
A holistic treatment plan addressing multiple symptoms and co-occurring disorders is often necessary. To that end, a teen with DID may undergo trauma-specific individual and group therapy in addition to taking medication to help reduce their symptoms.
An inpatient or outpatient facility can help provide structure in a teen’s treatment and give them the medical and psychiatric attention they need while providing a safe or comfortable home environment or allowing them to continue going to school and home between treatments.
For more information about dissociative identity disorder in teens, contact us today.
Visions Treatment Centers is here to help you get the quality treatment you deserve.