Dissociative disorders have a relatively high prevalence yet are also easily one of the most misunderstood psychiatric conditions in the general public’s eyes. Dissociative disorders are characterized by a disconnection from reality following a traumatic experience. Dissociation in a clinical sense can take on many different forms – but it is best described as a state of mind that allows a person to break away from the past and present and become separated from their pain.
Unfortunately, the overwhelming majority of people with a dissociative disorder have an additional psychiatric diagnosis, from depression or anxiety to substance abuse. According to data pulled from several countries, dissociative disorders are estimated to affect about 1 to 5 percent of the general population. One study on teens seeking help at an outpatient psychiatric facility estimated that as many as 45 percent were struggling with a dissociative disorder of some form.
What Is a Dissociative Disorder?
Dissociative disorders are a class of conditions defined as problems with the following:
-
- Memory
- Identity
- Emotion
- Perception
- Behavior
- Sense of self
In a sense, mild dissociation is a common occurrence, one most people experience. For example, many of us may have daydreamed at some point, gotten lost in our thoughts, or experienced a form of “highway hypnosis.” However, dissociative disorders describe behavior and symptoms that are much more severe.
Dissociative disorders are pervasive across settings and disrupt nearly every aspect of life. Teens struggling with a dissociative disorder aren’t just aloof. Still, they may appear completely changed after a traumatic event, to the point that they seem like a different person, either due to the coping behaviors they’ve adopted or due to lapses and holes in their memory.
Types of Teen Dissociative Disorders
Dissociative disorders are split into three different diagnoses:
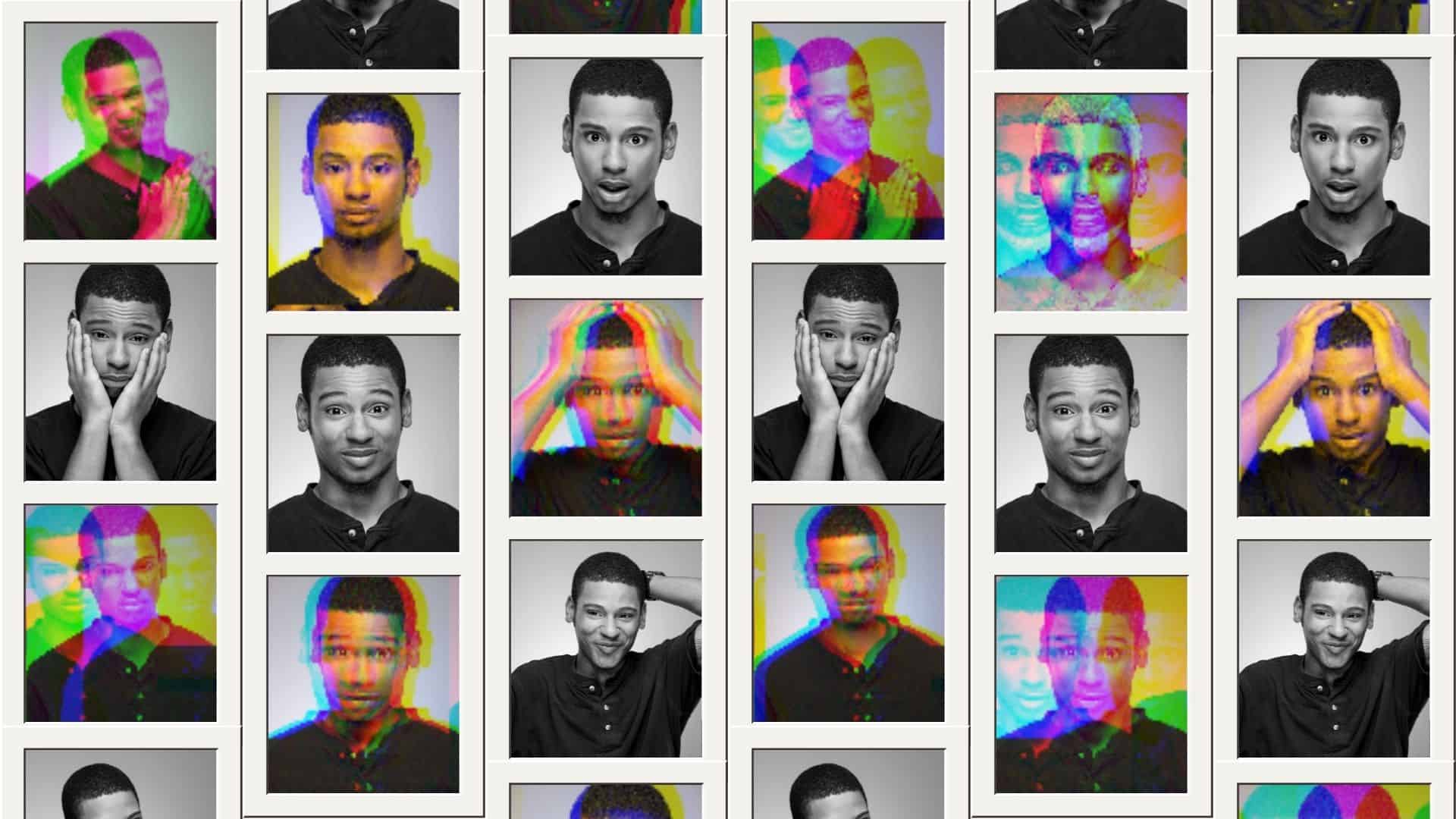
Dissociative Identity Disorder (DID)
In cases of dissociative identity disorder (DID), previously known as multiple personality disorder (MPD), a teen will switch between two or more enduring personalities. These are not just different behaviors but give the impression of being several distinct people. However, in DID cases, a teen is not actually inhabited by multiple persons or “alters” but has instead constructed different personalities to cope with their past.
Sometimes, these personalities are not necessarily human. Instead, they may each have their own set of memories. The overwhelming majority of people diagnosed with DID have experienced overpowering and often recurring trauma, usually before age 6. While dissociative disorders may be more common than we suspect, rates for DID remain around 1 percent. Another major symptom is gaps in memory, far more than regular forgetfulness.
Dissociative Amnesia (DA)
Dissociative amnesia (DA) is a more common form of dissociation and may involve blocking out information that would otherwise be consciously available after a traumatic event. However, such information would often still be subconsciously affecting one’s behavior and decision-making. For example, someone who was victimized in a closet may have an intense aversion towards opening closets or being inside them without remembering why.
Dissociative amnesia is usually diagnosed after trauma, in cases where gaps in memory or amnesia cannot be explained by another potential cause (such as brain trauma, intoxication, or the intake of certain memory-affecting substances (including surgical anesthetics). Dissociative amnesia is often either localized (not being able to recall an entire event or period), selective (not being able to recall certain portions of an event or period) or generalized (not being able to remember anything about themselves and their history).
Depersonalization/Derealization Disorder (DPDR)
Teens diagnosed with depersonalization/derealization disorder (DPDR) are either experiencing symptoms of feeling like they’re living life in the third person, from someone else’s perspective (depersonalization), or they might seem intensely aloof, isolated, and disconnected from the world around them (derealization).
As with other dissociative disorders, DPDR is often the result of trauma but can occur alongside neurological problems such as seizure disorders or neurological damage after prolonged drug use (particularly hallucinogens, marijuana, or ketamine). Most DPDR symptoms are experienced episodically rather than consistently. They are recurring over the years, however, and onset is usually around age 16.
Other conditions may feature depersonalization or dissociation as part of their list of symptoms (schizophrenia and other psychotic disorders) and others closely related to dissociative disorders (acute and post-traumatic stress disorder).
Recognizing Teen Dissociative Disorders
Your teen may be experiencing a dissociative disorder if they often display severe gaps in memory, seem to be mentally somewhere else, have suddenly become emotionless at times, seem disconnected from reality, appear to be switching between distinct personalities, or are behaving very strangely, moving around almost automatically, and describing themselves as having no control.
Dissociative disorders can be difficult to treat, and a professional diagnosis is always needed before a treatment plan can be formulated. In addition, most teens with a dissociative disorder are also struggling with a co-occurring mental health condition, including depression, anxiety, stress disorders, or drug use. These co-occurring disorders can make treatment more difficult – but a holistic plan can help address them as well through a combination of talk therapy, pharmacology, and long-term care.
Teen Dissociative Disorders and Substance Abuse
Substance use disorder (SUD) is one of the most common co-occurring disorders among teens with dissociative disorders, in part because certain drugs can help teens better cope with their experiences. A case of SUD coupled with another mental health issue is often called a dual diagnosis. However, drugs are poor coping mechanisms and carry with them a slew of physical and mental downsides ranging from long-term organ damage to cognitive impairment, further memory problems, anxiety, and exacerbated dissociation.
How Are Teen Dissociative Disorders Treated?
Dissociative disorders are treated through a combination of trauma therapies, talk therapies, and medication in cases where co-occurring disorders require them. Unfortunately, there are no medications that effectively treat symptoms of dissociation. In some cases, a doctor may prescribe an antipsychotic drug, but most drugs prescribed to patients with dissociative disorders are antidepressants.
The bulk of treatment plans relies on cognitive-behavioral therapy (CBT) based therapies and modalities. It can take several months for therapists to successfully help their teen patients reintegrate into their lives, reclaim different elements of their identity, and lead a more fulfilling life. Finding ways to cope healthily with the past is vital to the process and success of long-lasting recovery. Family and friends play a critical role herein and provide the fundamental backbone for long-term treatment as the teen’s support system.